The latest media/public health fear/panic lie is that flu hospitalizations are at a record high. That’s the line on all the network shows that featured Fauci over the weekend, and on PBS, NPR, CNN, etc. It is completely false.
Here is a version of the lie from the pandemic’s most illustrious villain, who appears to be hoping for more school closures:
Our country is facing a tridemic: flu, RSV and COVID. "More than three-quarters of pediatric hospital beds nationwide are occupied, seniors are hospitalized at a higher rate for respiratory illness & flu hospitalizations are at a decade-level high." https://t.co/mjSUQ02VCN
— Randi Weingarten 🇺🇦🇺🇸💪🏿👩🎓 (@rweingarten) November 27, 2022
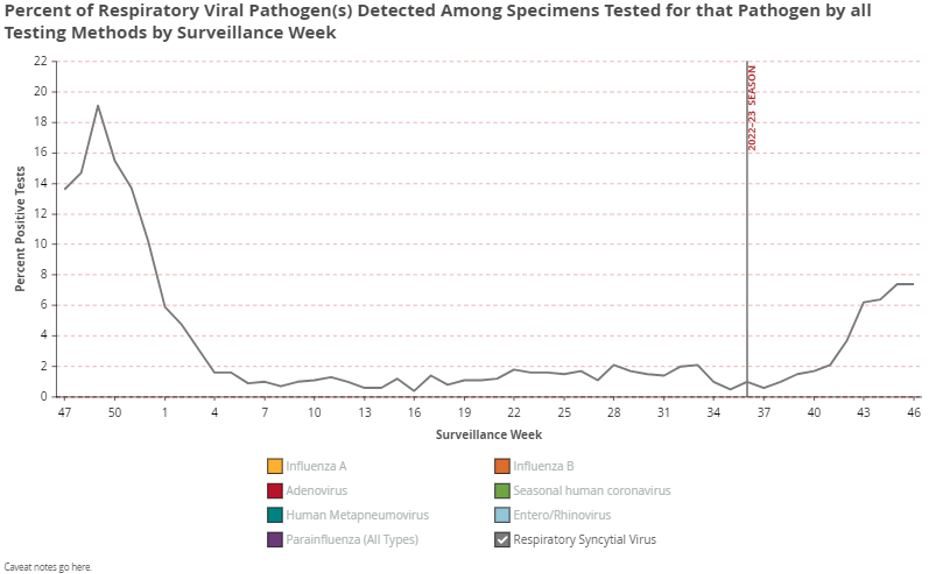
The truth is flu season is early by about six weeks, but otherwise looks completely normal. Here is the percent positive curve with a 6-week offset, compared to recent years:
CDC has posted flu view for Week 46, ending November 19, 2022. Clinical labs printed 18.2% positive. Here is that offset 6 weeks plotted with recent years. pic.twitter.com/lEHL1JIl36
— Phil Kerpen (@kerpen) November 28, 2022
But there is no evidence that an earlier flu season is more severe.
As the CDC’s data shows, flu hospitalizations are nowhere near a high compared to any recent pre-pandemic years and there is no apparent relationship between when a flu wave arrives and its severity. (The most recent data point reflects reporting lag, not a peak yet.)
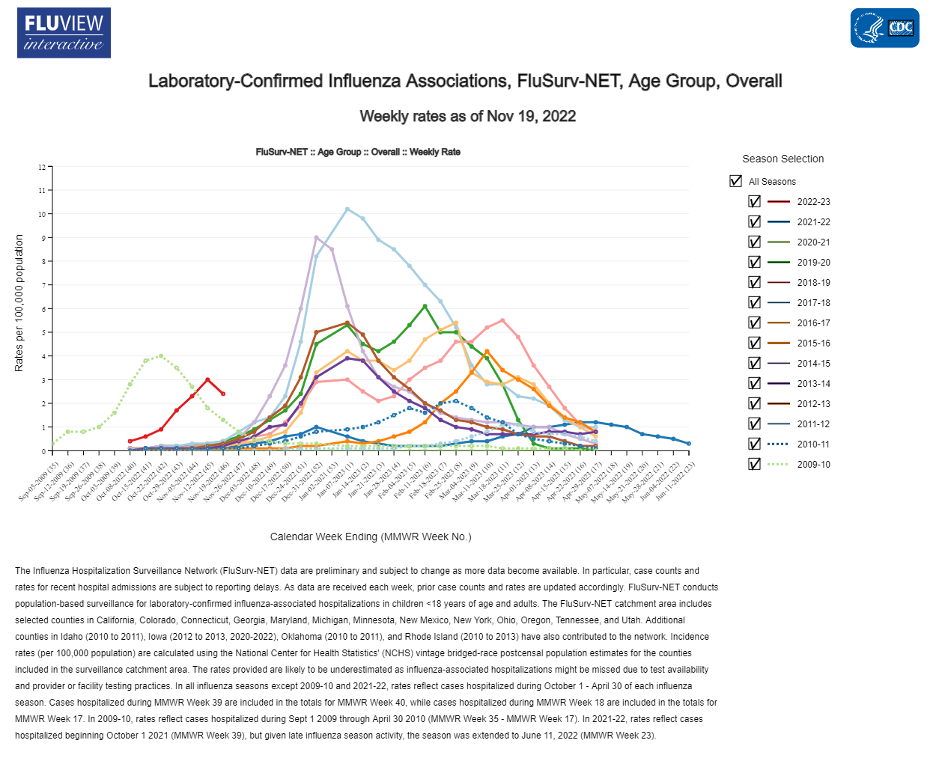
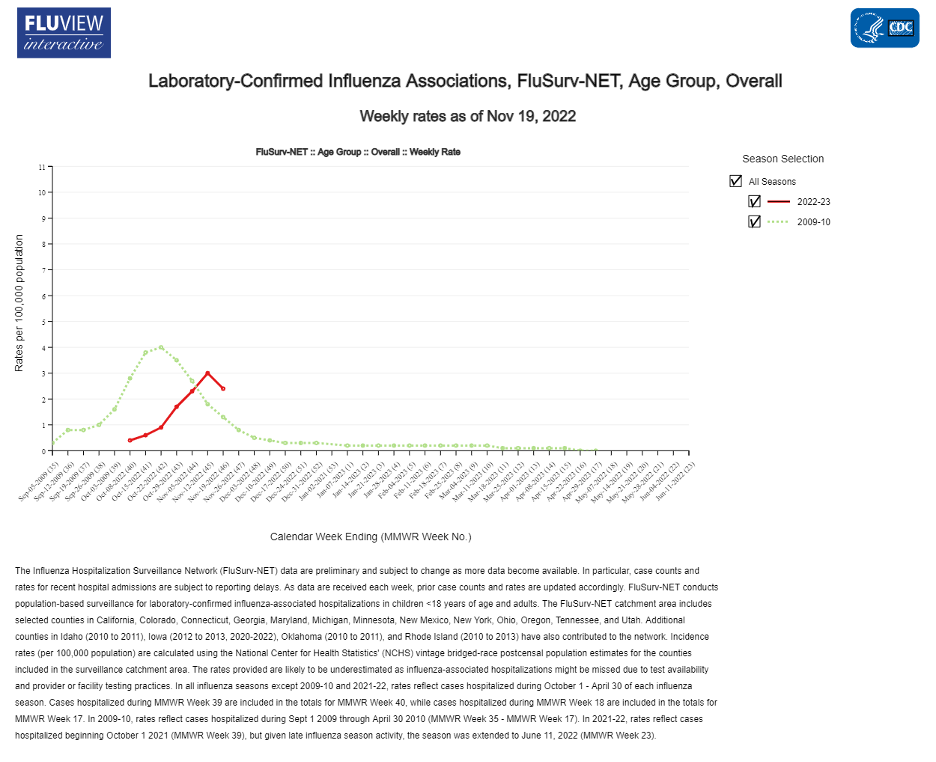
In fact, isolating the comparison of this year’s hospitalization curve to the last time flu arrived this early – the swine flu pandemic year of 2009 – shows that the last time flu was this early it was an unusually mild year, peaking low and early and declining toward zero for the duration of the usual season.
RSV returned last summer with a global out-of-season wave after a skipped season in the first pandemic year, and arrived this year in an out-of-season fall wave. This pattern occurred globally without respect to masks.
RSV in Japan (the world's most masked country), Sweden (the world's least masked country), and United States, all show:
— Phil Kerpen (@kerpen) November 28, 2022
2020-21 skipped.
2021-22 two quarters early.
2022-23 one quarter early.https://t.co/t4oJLnaw4Bhttps://t.co/WtT9l4FDk2 pic.twitter.com/zBVfYx68V2
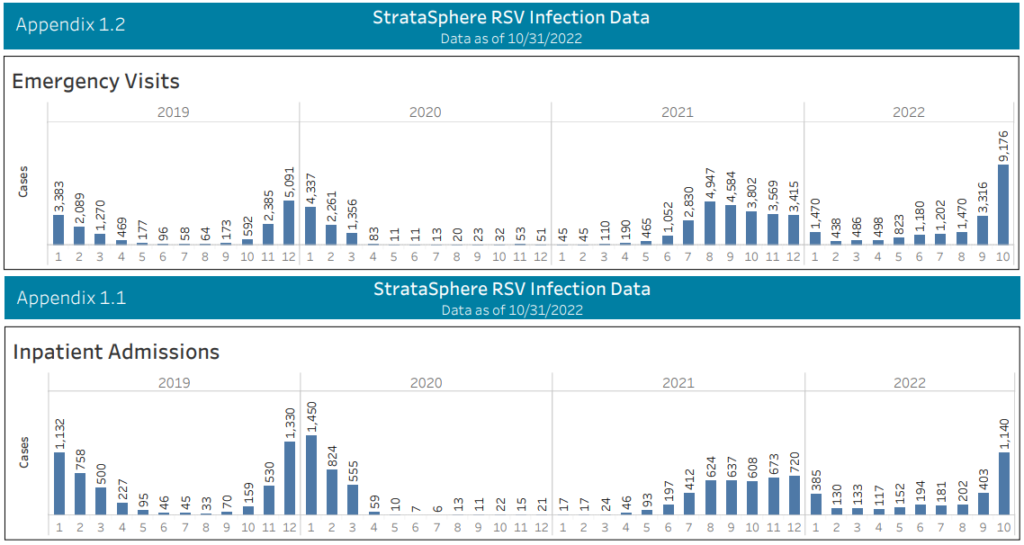
But other than the out-of-season timing, the RSV wave – now post-peak in at least 8 of the 10 HHS regions – was of typical magnitude.

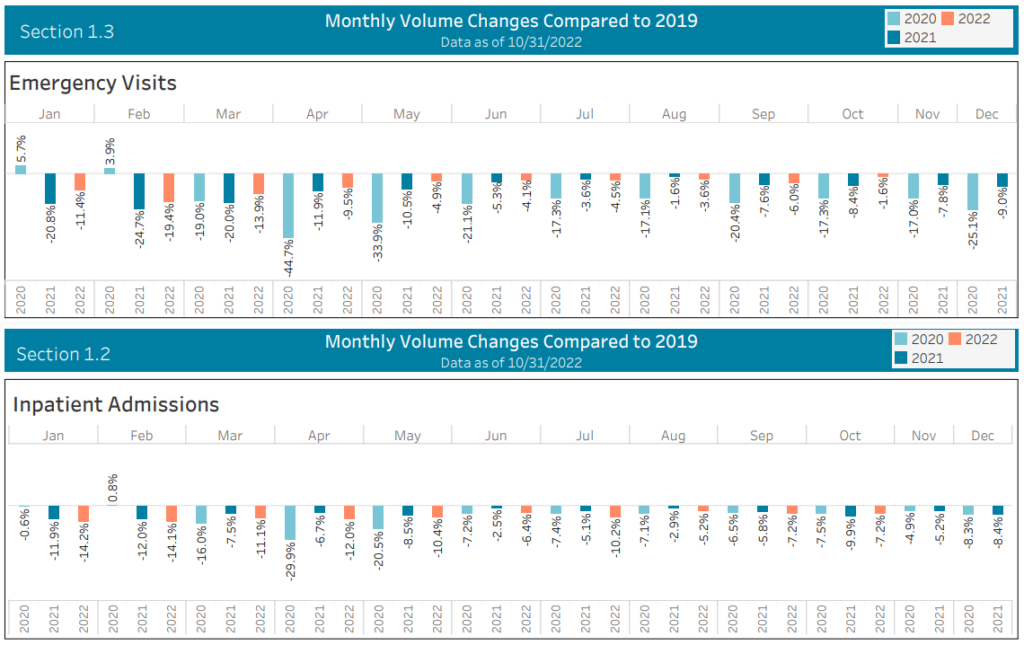
Hospitalization data from Strata shows that emergency visits were sharply higher in October than around the last RSV peak in winter 2019, but inpatient admissions were lower, suggesting a change in care-seeking probably driven by media hype:
Influenza disappeared globally at the outset of the pandemic and returned globally as COVID ceded ground without respect to masks or lockdowns – making the calls for imposing those measures for influenza ignorant as well as destructive.
Transcript of Dr. Osterholm on why the claim masks stopped flu is false and dangerous. pic.twitter.com/OfXb8xK0e5
— Phil Kerpen (@kerpen) October 22, 2021
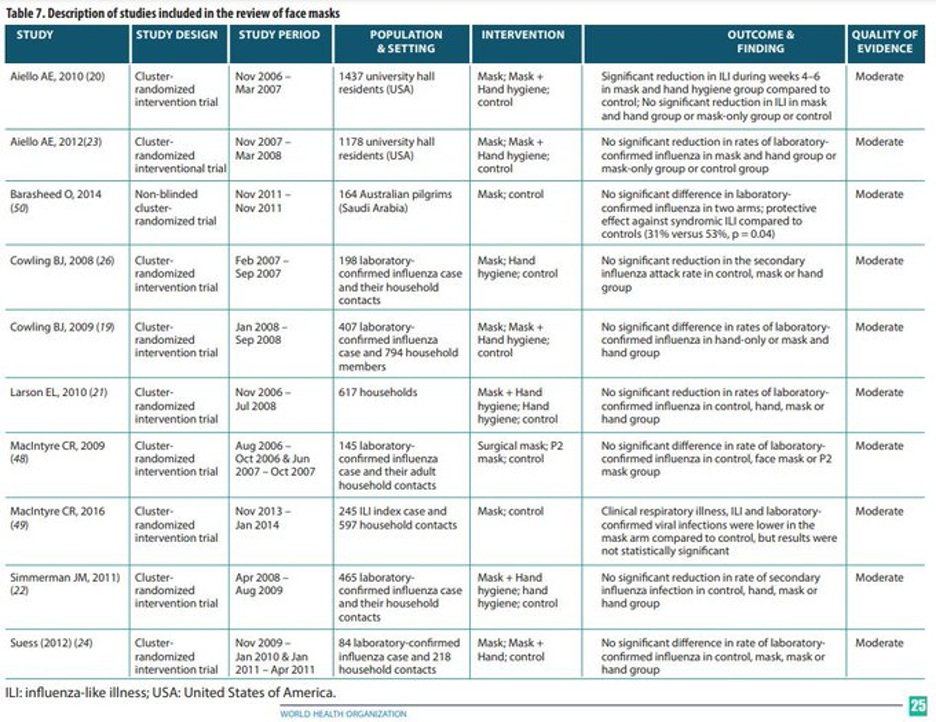
There are about a dozen randomized trials of masking for influenza, and all of them found no significant effect on transmission – although the narrative sections indicate the authors were trying awfully hard to find one. This is a very well-studied issue and proponents of masks cannot disregard empirical evidence with an appeal to “novelty” as they did with COVID.
There is only one published trial of masks for RSV and it found them ineffective. Notably, in Ontario, the place in North America with the most aggressive effort to reimpose mask mandates in the name of RSV, the current RSV percent positive is notably lower than last year’s peak when strict mask mandates were in place.
Top experts are now saying what we observed two years ago: SARS-CoV2 tends to compete with the other respiratory viruses. Per Science:
SARS-CoV-2 and other respiratory viruses often “interfere” with each other. Although waves of each virus may stress emergency rooms and intensive care units, the small clique of researchers who study these viral collisions say there is little chance the trio will peak together and collectively crash hospital systems the way COVID-19 did at the pandemic’s start.
“Flu and other respiratory viruses and SARS-CoV-2 just don’t get along very well together,” says virologist Richard Webby, an influenza researcher at St. Jude Children’s Research Hospital. “It’s unlikely that they will circulate widely at the same time.”
“One virus tends to bully the others,” adds epidemiologist Ben Cowling at the University of Hong Kong School of Public Health. During the surge of the highly transmissible Omicron variant of SARS-CoV-2 in Hong Kong in March, Cowling found that other respiratory viruses “disappeared … and they came back again in April.”
The best real-time viral surveillance data comes not from the CDC, which is lagged and uses different systems to track different viruses, but from the private company Biofire, a popular provider of a respiratory testing panels. Their latest print shows RSV well post-peak and influenza rising sharply as rhinoviruses decline from a large wave that coincided with back-to-school. SARS-CoV2 is rising slowly from an extended low plateau.
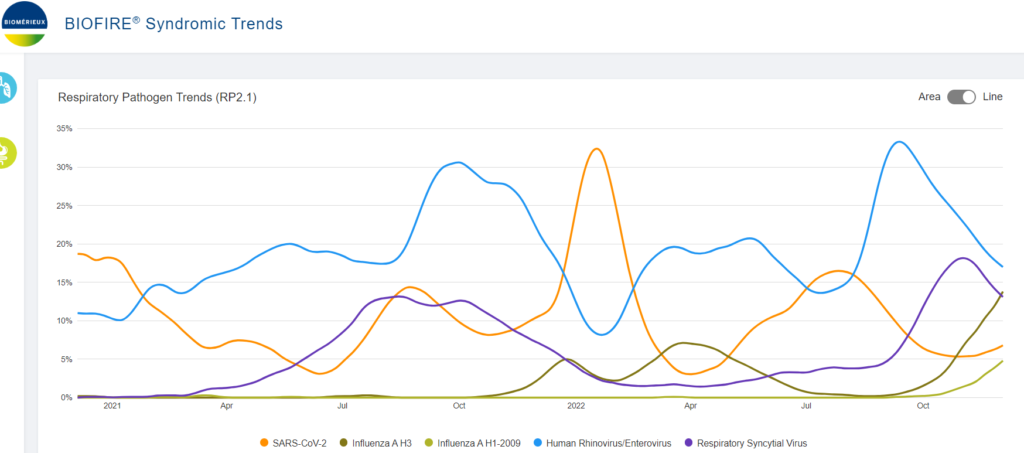
The RSV wave has already peaked around normal levels and the emergence this year of a normal epidemic flu wave is welcome news, indicating that the COVID pandemic is truly over and it is behaving like a normal respiratory virus.
The real hospital story – as we have reported throughout the pandemic but few others have – remains an underutilization story, with emergency department and inpatient volumes still failing to reach 2019 levels in any month since the pandemic started:
Here is another way to contextualize hospital utilization using the HHS Protect data and combining influenza hospitalization with COVID – the biggest movement has been the top lines, with a notable decline in total capacity and utilization.
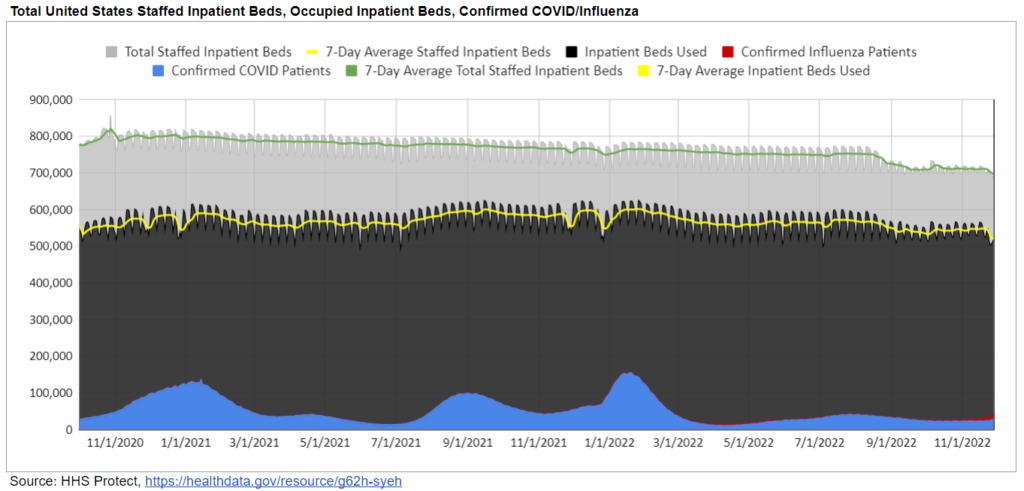
COVID is no longer dominant and that has allowed for a return of a normal flu wave. (And CDC reports that 100% of H3N2 flu sequenced by public health labs have been 3C.2a1b.2a.2 and are well-matched to this year’s flu shot.) That is fundamentally a good news story.
Attempts to stoke panic about RSV and flu by misrepresenting early timing as unusual severity should not be allowed to disrupt schools or businesses.
